Environmental factors highly impact training and racing. Learn the science behind acclimating to altitude, heat, humidity, and how air quality factors in.

Most of this content is from UESCA certifications and from UESCA advisor/contributor and physiologist, Corrine Malcolm, M.S.
There are a lot of unique things about endurance sports. However, perhaps one the most unique aspects is the influence of the environment on athletes. As an example, the Bob Cook Memorial Hill Climb (Mt. Evans) ascends 6,630 feet and tops out at a dizzying 14,130 feet! Whether it’s altitude, heat, humidity or cold weather; there are numerous environmental factors that influence endurance athletes both in training and in competition. As such environmental physiology and training considerations that are impacted by the environment are critical to understand for an endurance athletes.
Altitude
Since we were discussing the Mt. Evans hill climb, let’s start this post with altitude. Before we get into the acclimatization aspect of altitude, let’s first discuss some of the science behind altitude.
If you haven’t said it, you’ve probably heard it, “There’s no air up here!” But is that really the case? It turns out that even as you go up in elevation, say from sea level to the top of Pikes Peak (14,115 feet), the gases that make up the air around you remains the same, 20.93% oxygen (O2), 0.03% carbon dioxide (CO2), and 79.04% nitrogen). So if there isn’t “less oxygen” why do you feel so terrible? Well it turns out that as you go up in elevation, there is a decrease in partial pressure of oxygen, and your lungs rely on that partial pressure gradient for inhalation and exhalation. Additionally, that pressure gradient also influences gas exchange between your alveoli and capillary beds (1). So while there is not less oxygen, it’s a lot harder to get the oxygen both into your lungs and from your lungs into your circulatory system (and to your working muscles, brain, etc).
So how does your body adapt to not only survive but thrive at different elevations? When you arrive at higher elevations your body has to go through a series of adaptations incredibly quickly to counter your sudden decreased ability to transport oxygen efficiently (remember the pressure gradient from above?). Some of these adaptations take place very quickly within the first 24 hours at altitude, while others may take as long as several weeks to fully develop. So what are these changes?
Immediately your body tries to artificially boost the density of your red blood cells through a process known as haemoconcentration. This happens to temporally boost your hematocrit in hopes of transporting oxygen more effectively until your body can produce more red blood cells to help (2,3). This process however decreases your blood plasma volume by 10-25%. This is why your heart rate is generally elevated when you initially travel to altitude. Think about it, cardiac output (Q) = heart rate x stroke volume – and if your blood volume decreases (stroke volume) your heart rate has to increase to keep cardiac output stable. This is generally why athletes commonly feel worst between 24 to 72 hours after arriving at altitude.
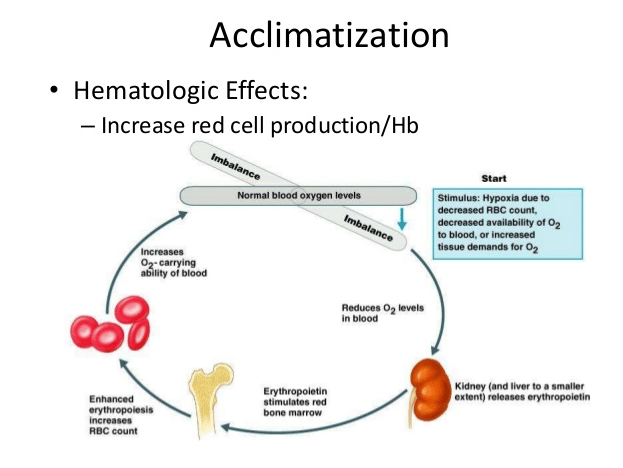
From the respiratory side, something occurs called a Hypoxic Ventilator Response. At altitude, because there is a decrease in O2 coming into your blood stream (again, remember the issue with the pressure gradient above?), your ventilation rate and depth of breathing increase. This ultimately shifts your pH balance, and if we know anything about the human body it’s that they like to operate in pretty finite windows. This shift in blood pH causes your kidneys to get involved, primarily via fluid balance from increased urination, in order to bring you back into equilibrium. This hypoxia induced pH shift does one more important thing, it triggers the release of more erythropoietin (EPO) (4). You might be thinking, EPO like the illicit drug? Well, yes, however EPO is also naturally produced to help stimulate the production of red blood cells. This process, called erythropoiesis, takes at least one week but as many as two to three weeks to allow red blood cells to mature and become fully functional. These long term changes ultimately lead to an expanded blood plasma volume, increased hematocrit and hemoglobin. This is the primary goal of altitude exposure, physiologically, the ability to carry more oxygen.
Altitude Acclimation Considerations

There’s a distinction to be made when thinking about altitude; are you trying to use altitude to improve general endurance performance or are you specifically trying to perform in an event at altitude? For most athletes, outside of elites with means for extended training camps (21-28 days in length), our primary concern is performing at altitude, (i.e., you’re from Wisconsin and will be competing at Leadville, CO). From there you need to consider several factors. These include: at what elevation do you live, at what elevation do you train, at what elevation is your event, and what means do you have to arrive at the event early?
The most basic recommendation for racing at altitude, based on what we know, is to arrive at least one week before race day. This is because the likelihood is that you:
1) Are past the ‘worst of it’ in the first 24-72 hours at altitude
2) Have already started to positively adapt to the higher elevation.
This is also why it’s often recommended if you cannot arrive at altitude early (at least one week) you are better off arriving the night before or morning of the event. Once again missing the ‘worst of it’ window before your body starts to work through incredibly taxing changes.
There are two primary types of altitude acclimation; the first is hypobaric hypoxia exposure (normal altitude exposure), the second is normobaric hypoxia exposure (simulated altitude exposure, think altitude tent). Both have been shown to work, but the key difference is a question of dosage, and potentially practicality. For hypobaric hypoxia, ie going to altitude, it appears the critical value for adaptation is having chronic exposure to elevations between 5,905 feet (1800 meters) to 9,842 feet (3000 meters) for ideally at least two weeks and up to four weeks to reap maximum benefits (red blood cell production/maturation) (5). It should be noted that going above 9,842 feet is not inherently negative, however it appears that there is no added benefit from an adaptation standpoint.
But what if you don’t not have the luxury to get away to altitude for that long? Enter, normobaric hypoxia exposure, or rather, the utilization of an altitude tent. It appears that the time course for adaptation remains about the same 3-4 weeks of accumulative time… but there’s the catch, accumulative time. When it comes to utilizing an altitude tent or room you are not actually spending 3-4 weeks in there, at most you are only getting 8-10 hours a day, and spending longer than that in bed veers dangerously towards bedrest which can have a negative impact on blood plasma volume. These things combined make the utilization of an altitude tent not as straight forward. Given the sheer volume of time that may be necessary in an altitude tent or room to produce adaptations, you need to weigh all the factors. These include the following:
- Can you afford the tent?
- Does it decrease the quality of your training by impacting your sleep quality?
- What elevation do you currently live at (there are more positive indications for altitude tents for those living closer to the minimum required altitude)?
- Is it possible that you can make it out to your race more than 72 hours prior to their event?
Use of Heat to Acclimate to Altitude
As having access to an altitude tent, or spending time at high altitude weeks in advance of a race are likely impractical due to cost and cost/time perspectives, respectively, it makes sense that other methods (cross-acclimation) to acclimate to altitude would be investigated and utilized.
While the use of heat acclimation training obviously makes sense for preparing for a race that will be hot, what about the use of heat acclimation training to prepare for races at altitude? This practice is getting attention due to some of the purported benefits. In other words, utilizing heat training stress to induce adaptations that are present at altitude. Of the main purported benefits, heat acclimation may reduce physiological strain at rest and during moderate intensity exercise at altitude – primarily via adaptations associated with improved oxygen delivery, increases in plasma volume and reductions in body temperature (6).
However, as this is an area of emerging research and due to the potential for stress on the kidneys, it is not advised at present time. However, this cross acclimation area should be paid attention to as more research and findings come out.
Heat

Like altitude, let’s start off with the physiology behind heat acclimation.
Although humans are uniquely suited for lots of complicated tasks, it turns out we are also inherently inefficient as well. For example, when it comes to ‘doing work’ like propelling yourself up a hill (and all the metabolic processes that make that happen), the majority of that work simply generates heat without having anywhere to go. To manage this, the body has its own thermostat, the hypothalamus, the thermoregulation center of the brain. It utilizes a negative feedback loop; when your skin and core temperature drops you experience vasoconstriction and shivering to keep warm blood near your core and produce heat. Conversely, when you heat up, you vasodilate – sending blood out towards the skin surface allowing heat to dissipate into the environment while activating sweat glands to utilize evaporative cooling.
As you exercise, there are two major factors that contribute to you heating up, the metabolic heat you are producing internally and the heat the environment applies to you externally. When it comes to environmental factors you will be impacted differently depending on where you are exercising. Some examples, including ambient air temperature is greatly influenced by the surface you are on, direct vs indirect sunlight, and even the direction of the wind.
These impact the four categories of heat transfer; conduction (direct transfer of energy), convection (air or water moving over your skin), radiation (direct or indirect transfer of sunlight), and evaporation (conversion of gas to liquid) (7).
All of these things work together to either heat you up or cool you off, but their effect is largely dependent on the temperature gradient between you and the surrounding environment, because even heat moves along a gradient (high to low concentration). A temperature gradient describes what direction and at what rate temperature changes for a particular location.
Heat Acclimation Considerations
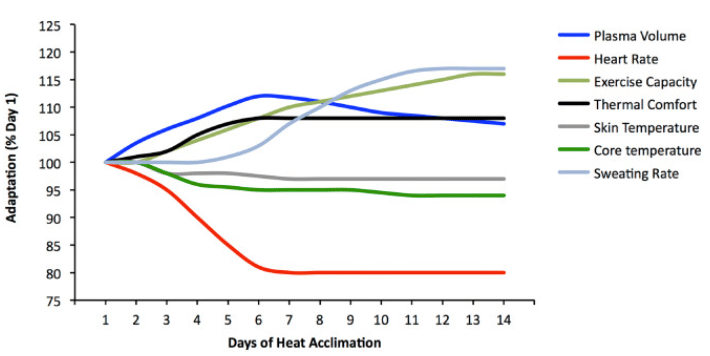
The human body is incredibly smart, and with chronic, daily heat exposure your body can make changes that allow you to thrive and survive in hot environments (and even benefit us in cooler environments). These adaptations include:
- Increase in sweat rate and a corresponding decrease in sweat concentration
- Lower skin and core temperature that comes with blood plasma volume expansion
- Lower heart rate during exercise (back to normal heart rate)
- Increased fluid and cardiovascular stability
- Decrease in the metabolic cost of exercise (8,9).
When you add up all these factors you have the most important adaptation of all, the ability to tolerate and feel more comfortable in the heat on race day. What’s really quite striking, compared to altitude acclimation, heat acclimation happens fairly rapidly with the bulk of adaptation occurring in 6-7 days and are complete by ~14 days of heat exposure (10).
Pre-race
When it comes to managing heat, it is advantageous to break it up into two main time periods, pre-race and during-race cooling. The pre-race period is the most effective way you can prepare for heat exposure. This happens naturally as you are exposed to warmer temps during spring and summer months, but that’s not always convenient (largely due to your training potentially not happening in warm enough temps based on location and time of year).
There are many physiological benefits of heat acclimation. Some of these benefits are as simple as jump starting your preparation for warmer temps, while others come from the positive effects of things like blood plasma volume expansion etc. So how does one heat acclimate?
It’s important right off the bat to get on board with one thing, you need to ask yourself, “how do I elicit the adaptation I want, with the lowest possible dose?” This is of utmost importance because anything you add to training is stress, and whenever you add additional stress there will always be possible tradeoffs. ie, what do we have to remove to make room for the additional stress we are adding. From the literature it is clear that daily increases in core body temperature through exercise in warm temps, environmental stress, passive heat interventions (sauna or hot water immersion), or a combination of the above will induce a meaningful physiological change that will ultimately increase thermal tolerance (881). However, when it comes to what is best for you, it boils down to what do you have at your disposal and what can you tolerate.
The methods that are most commonly used by athletes include:
- Natural heat acclimatization (exercising in a natural warm environment)
- Controlled hyperthermia (overdressing)
- Controlled intensity (via exercise in climatic chamber)
- Passive heating (post exercise heating via sauna or hot water immersion) (11).
As mentioned above, all of these methods work, but they all require different doses to elicit change. This is because the physiological tipping point requires your core body temperature to reach ~101F (38.5C) for approximately 90 minutes. It should be noted that more is not better; more time in a session is not better, twice a day is not better, weeks on end is not better. So where does that leave us?
Of the methods mentioned, you have to ask yourself which one maintains your ability to maintain the highest quality training and add the least amount of additional workload? Methods like overdressing or training in a climatic chamber often mean sacrificing the quality of the individual workouts by having to cut down the volume or intensity. Traditional time in a dry sauna, steam room, or hot tub require a lot of additional time added to your day, 60-90 minutes on top of normal training, that might not be manageable. So in considering your needs, not impairing your training, and the dose needed, passive heating which combines heat exposure immediately post exercise rises to the top of this pile. Why is that? Because you are allowing yourself to maintain the quality of their workouts by training in their natural environment, and also spend less time in the actual heat because you go into the heat exposure ‘pre-warmed’ from exercising. This means suddenly you only have to spend 20-30 minutes in the sauna instead of 60-90 minutes, which is both easier on the body, and also easier to manage from a time perspective.
Cooling During a Race

We’ve talked about prepping pre-race from an acclimation standpoint, but what about the other pieces of this puzzle? You’ve done the work, you’re fit and as ready as you can possibly be, so what other strategies can you employ to mitigate heat-related issues on race day?
In shorter races there are some pre-race cooling strategies you can try to utilize – these generally include trying to preemptively lower core body temperature to allow for extra heat storage capacity. However, ultras are generally considered too long for something like this to be effective. This leads us to during-race cool strategies. The goal of these strategies is to help rapidly remove excess heat from the body. Unlike pre-cooling, the purpose of during-race cooling is not so much about actually lowering core body temperature, but to keep skin temperature low enough to allow a temperature gradient to be present which helps to move heat out into the environment by promoting vasodilation.
Suggested strategies to employ are:
- Packing ice on your torso, icing your neck and head (via ice bandanas, ice collars and special ice hats)
- Icing your peripheral arteries (putting ice down arm sleeves)
- Wearing loose and light-colored clothing
- Limit conductive heat (avoid dark colors)
- Increasing evaporative cooling (getting wet)
- Drinking cool fluids (12,13).
Other Heat Acclimation Information and Considerations
- Individuals will differ greatly in their ability to deal with heat and humidity.
- The more body fat an individual has, the less efficient they will be at dissipating body heat.
- Generally, the larger the individual, the more energy is required to reduce body heat. This is because the smaller the individual, the larger the skin surface compared with body volume. This enables small individuals to dissipate heat better than large individuals (14).
- Wind speed, humidity, and shade all affect an individual. Sweat must evaporate to cool the body. Therefore, in humid conditions where sweat does not evaporate as well as in non-humid conditions, the chance for overheating increases.
- After 10 days of heat acclimatization, the capacity for sweating nearly doubles (15).
- Novice endurance athletes and deconditioned individuals are often the most negatively affected by hot weather.
- The physiological benefits of heat acclimatization are lost between two and three weeks post-acclimation training(594).
- Individuals who are heat acclimatized can sweat up to 4 liters/hour, while those who are not acclimatized will sweat approximately 1.5 liters/hour (16). This demonstrates the increased efficiency regarding thermoregulation due to heat acclimatization training.
Humidity

But what about humidity? As anyone who has experienced humidity can tell you it makes everything feel harder, and there is some truth to that. This is because it hampers your primary mode of getting rid of heat via evaporative cooling. Remember heat and moisture, among other things, want to move along a gradient from areas of high concentration to areas of lower concentration. Just as this is true of heat, it’s easier to cool off when the temperature is lower than core and skin temperature, it is true for sweat (or any moisture) as well. For evaporative cooling to work there needs to be ‘room’ for that to happen, ‘room’ for that moisture to move from your skin and into the air taking heat along with it from your body. When the humidity creeps your ability to utilize evaporative cooling from either sweat or other water (from ice melt or water you’ve dunked in) leaving the surface of your skin goes down.
So humidity doesn’t only make everything feel harder, it makes everything harder. This has led some to believe that it’s important to acclimate to the type of heat you might be exposed to on event day (humid vs dry heat). However, there is concern that adaptation to humid heat (via steam rooms etc) might actually blunt your sweat response as it is not as useful in those environments. Because of this, try sticking with a traditional dry heat acclimation with the option to add in some supplementary sessions in a humid environment primarily to build tolerance to it.
Environmental Conditions and Lung Health
Frequent seasonal questions have to do with when it is or isn’t a good idea to exercise outside. This could be in the winter months as temperatures plummet or during fire season that drops air quality for days to weeks on end. Now these conditions effect everyone differently and most of us will have our own personal threshold for temperature or air quality, but the likelihood is we’ve all gone for a run or ride at some point in conditions we shouldn’t have. Be it cold or dry air, or air high in particulate matter (from diesel exhaust or wild fire smoke) both are taxing on your lungs and can lead to a breathing condition like exercise induced bronchospasm (EIB) formerly called both exercise induced asthma and hyper-reactive airway.
EIB is not an acute condition, ie it’s generally not a one-off event, but one that is caused from chronic exposure to something. In many respects, it could be referred to as an overuse injury. The cells that make up the lining of your airways are incredible in that they can repair themselves quickly. However, with repeated injury and repair they can become maladapted as well, becoming more reactive overtime. While at rest your ventilation rate is only 12-20 breaths per minute, but while running you may be breathing at a rate of 50 breaths per minute or more. It’s this increase in ventilation combined with an irritant (ie cold, dry, or polluted air) that exposes athletes to more risk. So while you are breathing, and breathing hard, you cause water to evaporate from the airway liquid surface that lines your bronchioles at a rate that you cannot keep up with. This drying then causes a shift in the osmotic gradient (again a gradient) in the cells that makeup the airway which stimulates the release of inflammatory mediators. These inflammatory mediators, such as histamine, act on the smooth muscles of the bronchioles causing constriction, mucus buildup, and edema (swelling) of the bronchioles.
As mentioned above, this is not an acute problem, but rather a slow and progressive one that worsens over time. One day of training in extreme cold or smoky skies will not guarantee you a lifetime of breathing issues, however continued training in them does heighten your risk. So what can you do to protect yourself and your lungs?
- You don’t lose fitness overnight. Fitness decay take two weeks of zero exercise to set in. So take a day off, or two, or three, and support your athlete in that. Their long term health is always more important.
- You can alter the plan. When air quality or temperature drops move the intervals inside or cut the intensity. Remember as ventilation increases, exposure also increases.
- Shorten the total duration. Not only is it how hard you are working but how long you are working. If you are staying outside, consider cutting the duration of the workout to limit exposure.
- Be flexible. For air quality or air temperature there are generally times of day that are better than others. Air quality tends to be worse midday and better early in the morning and later in the evening. Air temperature tends to warm as the day goes on, try to get intervals in during warmer afternoon periods during cold months.
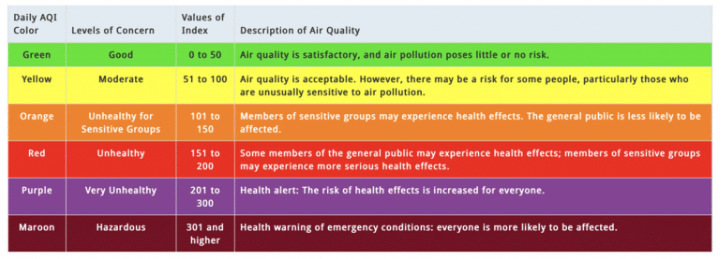
- Know your threshold. There is not one threshold for everyone, but with health in mind air on the side of caution. For cold temperatures you can use the international ski federation cut off of -4F (-20C). To be fair, this cut off is more to do with exposure (cold injury risk) and less about the lungs, and I would caution most athletes to move intervals inside when temperatures fall below 10F. If you are coughing after a hard workout that is generally a side effect of drying of that airway surface. For air quality I’d encourage you to avoid intervals if AQI is above 75 (unless you have a history of asthma, then threshold is lower), cut duration of workout if air quality is between 100-150, and avoid outside exercise if air quality is above 150.
Summary
So there you have it – the nuts and bolts of environmental physiology and the related training and racing considerations. I hope that you enjoyed this content and hopefully it will make your next race in the heat or altitude a bit more palatable!
Corrine Malcolm is an advisor and contributor to UESCA. Corrine holds a BS in Exercise Physiology from Montana State University-Bozeman and a MS in Environmental Physiology from Simon Fraser University. Corrine is a former US Biathlon national team athlete and is currently a professional ultrarunner for Adidas-TERREX. Additionally, she is also a coach and science writer.
- Sinex, J. A., & Chapman, R. F. (2015). Hypoxic training methods for improving endurance exercise performance. Journal of Sport and Health Science,4(4), 325-332. doi:10.1016/j.jshs.2015.07.005
- Beidleman, B. A., Fulco, C. S., Cadarette, B. S., Cymerman, A., Buller, M. J., Salgado, R. M., . . . Muza, S. R. (2017). Is normobaric hypoxia an effective treatment for sustaining previously acquired altitude acclimatization? Journal of Applied Physiology,123(5), 1214-1227. doi:10.1152/japplphysiol.00344.2017
- Chawla, S., & Saxena, S. (2014). Physiology of high-altitude acclimatization. Resonance,19(6), 538-548. doi:10.1007/s12045-014-0057-3
- Anderson, J. (2018, May 20). Acclimatization To Altitude. Retrieved from https://www.jenreviews.com/acclimatization-to-altitude
- Constantini, K., Wilhite, D. P., & Chapman, R. F. (2017). A Clinician Guide to Altitude Training for Optimal Endurance Exercise Performance at Sea Level. High Altitude Medicine & Biology,18(2), 93-101. doi:10.1089/ham.2017.0020
- Gibson OR, Taylor L, Watt PW, Maxwell NS. Cross-Adaptation: Heat and Cold Adaptation to Improve Physiological and Cellular Responses to Hypoxia. Sports Med. 2017;47(9):1751-1768. doi:10.1007/s40279-017-0717-z
- Sawka, M. N., Leon, L. R., Montain, S. J., & Sonna, L. A. (2011). Integrated Physiological Mechanisms of Exercise Performance, Adaptation, and Maladaptation to Heat Stress. Comprehensive Physiology,1883-1928. doi:10.1002/cphy.c100082
- Rivas, E., Rao, M., Castleberry, T., & Ben-Ezra, V. (2017). The change in metabolic heat production is a primary mediator of heat acclimation in adults. Journal of Thermal Biology,70, 69-79. doi:10.1016/j.jtherbio.2017.10.001
- Périard, J. D., Racinais, S., & Sawka, M. N. (2015). Adaptations and mechanisms of human heat acclimation: Applications for competitive athletes.
- Minett, G. M., Skein, M., Bieuzen, F., Stewart, I. B., Borg, D. N., Bach, A. J., & Costello, J. T. (2016). Heat acclimation for protection from exertional heat stress. Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd012016
- Daanen, H. A., Racinais, S., & Périard, J. D. (2017). Heat Acclimation Decay and Re-Induction: A Systematic Review and Meta-Analysis. Sports Medicine,48(2), 409-430. doi:10.1007/s40279-017-0808-x Daanen, H. A., Racinais, S., & Périard, J. D. (2017). Heat Acclimation Decay and Re-Induction: A Systematic Review and Meta-Analysis. Sports Medicine,48(2), 409-430. doi:10.1007/s40279-017-0808-
- Tyler, C. J., Sunderland, C., & Cheung, S. S. (2013). The effect of cooling prior to and during exercise on exercise performance and capacity in the heat: A meta-analysis. British Journal of Sports Medicine,49(1), 7-13. doi:10.1136/bjsports-2012-091739
- Bongers, C. C., Hopman, M. T., & Eijsvogels, T. M. (2017). Cooling interventions for athletes: An overview of effectiveness, physiological mechanisms, and practical considerations. Temperature,4(1), 60-78. doi:10.1080/23328940.2016.1277003
- O’Connor H, Olds T, Maughan RJ; “Physique and performance for track and field events.” J Sports Sci. 2007;25 Suppl 1:S49-60.
- Costill DL, Branam G, Fink W, Nelson R. “Exercise induced sodium conservation: changes in plasma renin and aldosterone.” Med Sci Sports. 1976 Winter;8(4):209-13.
- Brooks GA, Fahey TD, Baldwin KM. “Exercise Physiology: Human Bioenergetics and its Applications.” 4th edn. New York: McGraw-Hill; 2004.








